TACE vs TARE for Liver Cancer: A Comprehensive Comparison
Liver cancer is a complex and challenging disease to treat, requiring a multidisciplinary approach and advanced therapeutic techniques. Two of the most prominent Interventional radiology treatments for liver cancer are Transarterial Chemoembolization (TACE) and Transarterial Radioembolization (TARE).
These minimally invasive procedures offer targeted treatment options that can significantly improve patient outcomes.
Dr. Amit Sahu, amongst leading Interventional radiologist in Mumbai, specializes in these procedures, providing patients with access to advanced liver cancer treatments.
This blog will explore the differences between TACE and TARE, their effectiveness, and how to choose the right treatment.
Understanding TACE (Transarterial Chemoembolization)
What is TACE?
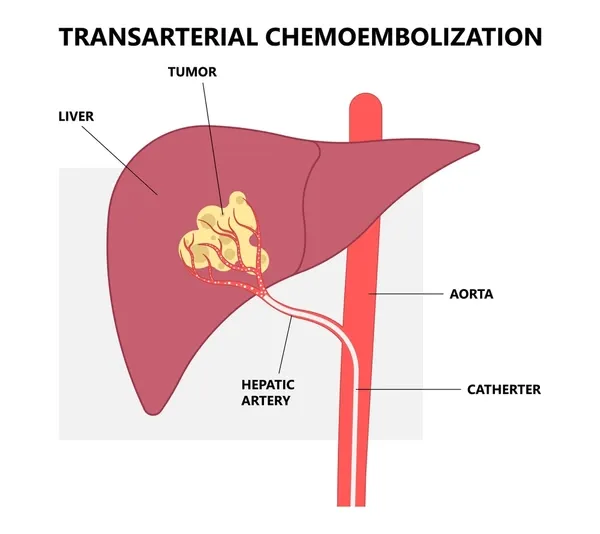
Transarterial Chemoembolization (TACE) is a targeted therapy for liver cancer that involves delivering high doses of chemotherapy directly into the liver tumor. This is done through a catheter inserted into the blood vessel (artery) which supplies blood to the tumor.
The procedure also involves blocking the blood flow to the tumor by injecting embolic agents, effectively trapping the chemotherapy within the tumor.
- Localized Treatment: TACE targets the tumor directly, minimizing the exposure of healthy tissues to chemotherapy.
- Dual Action: Combines the effects of high-dose chemotherapy and ischemia (lack of blood supply) to enhance tumor destruction.
- Minimally Invasive: Performed through a small incision, reducing recovery time and risk of complications.
Indications and Patient Suitability for TACE
TACE is particularly effective for patients with liver cancer who are not candidates for surgery or interventional ablative therapies, either due to the location of the tumor or being larger in size or underlying health conditions.
- Ideal Candidates: Patients with intermediate-stage liver cancer, those with tumors that are too large for ablation, or those awaiting liver transplantation to help keep good tumor control and maintain in list.
- Contraindications: Patients with severe liver dysfunction or extensive tumor spread beyond the liver may not be suitable for TACE.
Procedure and Recovery
The TACE procedure typically involves the following steps:
- Preparation: Patients undergo imaging and tests to assess liver function, tumor characteristics, number, location and extent of tumor.
- Catheter Insertion: A catheter is inserted through a small incision in the groin or wrist artery and guided to the artery supplying the liver tumor.
- Chemotherapy Delivery: Chemotherapy drugs are delivered directly into the tumor, followed by embolic agents to block blood flow.
- Post procedure Care: The procedure usually takes a few hours, and patients may need to stay in the hospital overnight for observation.
- Recovery Time: Most patients can return to normal activities within a week, though they may experience mild side effects such as fatigue, nausea, or pain.
- Effectiveness Duration: TACE can be effective for several months (usual survival benefit of over 12-24 months), but the duration varies depending on the tumor’s response, underlying liver disease, etc.
- Follow Up: A scheduled regular follow up is done with blood tests and imaging to assess the response to therapy and plan further treatment.
Understanding TARE (Transarterial Radioembolization) or SIRT (Selective Internal Radiation Therapy)
What is TARE?
Transarterial Radioembolization (TARE), also known as selective internal radiation therapy (SIRT), is a procedure that involves delivering radioactive particles directly to the liver tumor. These particles emit radiation that kills cancer cells while sparing the surrounding healthy tissue. In contrast, chemotherapy is injected in TACE procedure.
- Targeted Radiation: Delivers radiation precisely to the tumor, minimizing damage to surrounding healthy liver tissue. The radiation is safe and does not penetrate very far, thus risk of exposure to others in not there.
- Radioactive Microspheres: Tiny radioactive beads (usually Yttrium-90) are used to deliver high-dose radiation internally.
- Minimally Invasive: Like TACE, TARE is performed through a small injection, making it less invasive than traditional surgery.
- Pre-Requisite for TARE: One important factor in selecting patients suitable for TARE is performing a pre-TARE Tc-99m MAA scan. This test mimics the radioactive beads and helps predict the amount of radiation that may possibly leak into the lungs. If the dose of leaked radiation is found safe, then it is considered safe to proceed with TARE treatment.
Indications and Patient Suitability for TARE
- TARE is typically recommended for patients with primary liver cancer or metastatic liver cancer who have not responded to conventional therapies. It has even been found useful in patients with various degrees of portal vein invasion.
- Ideal Candidates: Patients with inoperable liver cancer, those with tumors that are resistant to chemotherapy, or those who require a treatment option with fewer side effects. Patients with liver cancer awaiting transplant can also benefit from TARE to have tumor control.
- Contraindications: Patients with excessive lung exposure on pre-TARE scan, poor liver function or a high tumor burden may not be suitable for TARE.
Procedure and Recovery
The TARE procedure involves the following steps:
Preparation: Pre-procedure imaging and tests are conducted to map the blood vessels and assess liver function.
- Catheter Insertion: Similar to TACE, a catheter is inserted and guided to the hepatic artery.
- Radioactive Particle Delivery: The radioactive beads are delivered to the tumor, where they emit localized radiation over several days.
- Recovery: The procedure is typically outpatient, with patients returning home the same day.
- Recovery Time: Most patients experience minimal discomfort and can resume normal activities within a few days.
- Effectiveness Duration: The radiation continues to work over several weeks, with the effects lasting for months.
Comparing TACE and TARE
Which is Better, TACE or TARE?
Choosing between TACE and TARE depends on various factors, including the tumor’s size, location, patient’s overall health, and specific treatment goals.
- Effectiveness: Both TACE and TARE have been shown to effectively shrink tumors and improve survival rates, but TARE is often preferred for larger or more resistant tumors.
- Side Effects: TACE is associated with side effects such as post-embolization syndrome (fever, pain, nausea), while TARE has fewer immediate side effects but requires careful patient selection due to the potential for delayed radiation injury.
- Recovery Time: TARE generally offers a quicker recovery with fewer side effects compared to TACE.
Choosing the Right Treatment for Liver Cancer
Consultation with a Specialist
Selecting the right treatment requires a thorough consultation with an experienced Interventional radiologist like Dr. Amit Sahu.
- Personalized Assessment: Dr. Sahu evaluates each patient’s case individually, considering factors such as tumor characteristics, overall health, and treatment goals.
- Informed Decision: Patients are provided with comprehensive information to make an informed decision about their treatment options.
Multidisciplinary Approach
Liver cancer treatment often requires a team of specialists, including oncologists, radiologists, hepatologist and liver surgeons, to develop the most effective treatment plan.
Collaborative Care: Dr. Sahu works closely with other healthcare providers to ensure that patients receive the most appropriate and effective treatment.
Accessing TACE and TARE in Mumbai
Dr. Amit Sahu offers both TACE and TARE treatments in Mumbai, providing patients with access to advanced liver cancer care.
- Leading Expertise: With extensive experience in interventional radiology, Dr. Sahu is well-equipped to perform these complex procedures with precision and care.
- Comprehensive Care: Patients receive personalized care, from initial consultation to post-procedure follow-up, ensuring optimal outcomes.
Conclusion
TACE and TARE are two of the most effective Interventional radiology techniques for treating liver cancer where surgery or ablation may not be suitable.
Each offers unique benefits and is suited to different patient profiles and tumor characteristics. Consulting with a specialist like Dr. Amit Sahu is essential to determine the best treatment option for your specific case.
If you are seeking liver cancer treatment in Mumbai, Dr. Sahu’s expertise in TACE and TARE can provide you with the best possible care.
FAQs
Q. What are the risks associated with TACE and TARE?
Both procedures carry minimal side effects, such as post procedure fever, pain, nausea and transient liver dysfunction due to damage to surrounding normal liver tissues. But these are generally low and managed with proper care, medications and are self limiting.
Q. Can TACE or TARE be combined with other treatments?
Yes, both treatments can be used alongside other therapies such as systemic chemotherapy, radiation therapy, or surgery.
Q. How do I prepare for a consultation about liver cancer treatment?
Bring your medical history, imaging results, and a list of questions to discuss with your specialist.
Q. What should I expect in terms of follow-up care after TACE or TARE?
Regular follow-up appointments are essential to monitor the effectiveness of the treatment and manage any side effects. Usually blood investigations and imaging is performed to assess the response.